JOURNALS || Health & Medicine Blog (ASIO)
BACKGROUND
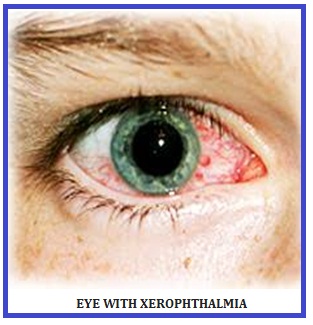
The term xerophthalmia covers all the ocular manifestations of vitamin A deficiency. Xerophthalmia can progress to irreversible blindness if left untreated. In endemic areas, vitamin A deficiency and xerophthalmia affect mainly children (particularly those suffering from malnutrition or measles) and pregnant women.
Disorders due to vitamin A deficiency can be prevented by the routine administration of retinol. Your body doesn’t produce vitamin A on its own. Instead, you have to get vitamin A from the foods you eat. Vitamin A is essential for vision because it’s an element of the protein that absorbs light in the receptors in your retina. Vitamin A is also important for the function and maintenance of your heart, lungs, kidneys, and other organs.
Even today, Xerophthalmia is a major problem in developing countries and is a leading cause of preventable blindness
SYMPTOMS
Night blindness is often the first evidence of vitamin A deficiency; the individual has a reduced ability to see in dim light.
The next sign is drying of the conjunctiva, which is known as conjunctival xerosis. Patches of xerosis give the appearance of sandbanks at receding tide. The conjunctiva loses its shiny luster and often becomes thickened, wrinkled and sometimes pigmented.
Sometimes accompanying the conjunctival xerosis are Bitot's spots, which are usually triangular-shaped, raised whitish plaques that occur in both eyes. When examined closely they look like fine foam with many tiny bubbles. This foamy, sticky material can be wiped away. Bitot's spots in the absence of xerosis may have a cause other than vitamin A deficiency.
The next stage is corneal xerosis, drying of the corneal surface, which first appears hazy and then granular on simple eye examination. The drying is followed by a softening of the cornea, often with ulceration and areas of necrosis.
Keratomalacia (the last and most severe sign of xerophthalmia): softening of the cornea, followed by perforation of the eyeball and blindness (extreme care must be taken during ophthalmic examination due to risk of rupturing cornea)
VITAMIN A SOURCE
Vitamin A comes from animal sources, such as eggs, meat, fortified milk, cheese, cream, liver, kidney, cod, and halibut fish oil. However, all of these sources, except for skim milk that has been fortified with Vitamin A, are high in saturated fat and cholesterol.
The best sources of vitamin A are:
- · Cod liver oil
- · Eggs
- · Fortified breakfast cereals
- · Fortified skim milk
- · Orange and yellow vegetables and fruits.
Other sources of beta-carotene such as broccoli, spinach, and most dark green, leafy vegetables.
The more intense the color of a fruit or vegetable, the higher the beta-carotene content. Vegetable sources of beta-carotene are fat and cholesterol free. Fats help the absorption of retinol and the carotenes.
VITAMIN A REQUIREMENT
According to the National Institutes of Health (NIH), recommended daily allowances for vitamin A differ depending on your age and, in some cases, gender.
|
Age |
Male |
Female |
|
0–6 months |
400 mcg |
400 mcg |
|
7–12 months |
500 mcg |
500 mcg |
|
1–3 years |
300 mcg |
300 mcg |
|
4–8 years |
400 mcg |
400 mcg |
|
9–13 years |
600 mcg |
600 mcg |
|
14 years and older |
900 mcg |
700 mcg |
The NIH gives separate recommendations for pregnant or breast-feeding women.
|
Age |
Pregnancy |
Breast-feeding |
|
14–18 years |
750 mcg |
1,200 mcg |
|
19–50 years |
770 mcg |
1,300 mcg |
These recommendations are for people who are healthy and well-nourished. Your doctor may make different recommendations if you have a medical condition or a vitamin deficiency.
TREATMENT
Vitamin A supplementation to the general child population is part of the health programs in many developing countries. Nutritional supplementation, rehabilitation, and education constitute a three-pronged approach in the management of dietary Vitamin A deficiency.
All individuals with xerophthalmia (except pregnant women) should be treated with large oral doses of 200000 IU vitamin A according to the WHO guidelines. The age-specific dose should be given on the first and second days and again 2 weeks later. This applies to all stages of active xerophthalmia, including night blindness, Bitot's spots, and corneal lesions. Corneal xerophthalmia is a medical emergency and should be treated immediately on diagnosis and then patients should be referred to a hospital for further treatment as they often present complex problems. Topical application of antibiotic ointment (tetracycline or chloramphenicol) is recommended for corneal lesions to prevent secondary infection. In addition, patients should be provided nutritional support and medical therapy.
In pregnant women, treatment varies according to the stage of illness:
• Hemeralopia or Bitot's spots: 10 000 IU once daily or 25 000 IU once weekly for at least 4 weeks. Do not exceed indicated doses (risk of foetal malformations).
• If the cornea is affected, risk of blindness outweighs teratogenic risk. Administer 200 000 IU once daily on D1, D2 and D8.
2.https://apps.who.int/iris/bitstream/handle/10665/133705/WHO_NMH_NHD_EPG_14.4_eng.pdf;
jsessionid=A3EA10746006C52DB927A5D52569012E?sequence=1
3. https://www.healthline.com/health/eye-health/xerophthalmia#treatment
4. https://www.ncbi.nlm.nih.gov/books/NBK431094/
5. https://www.provisu.ch/en/most-frequent-diseases/vitamin-a-deficiency
6. https://www.sciencedirect.com/science/article/pii/B012227055X006180
7. https://www.sciencedirect.com/science/article/pii/B9780723623038500159